If you’ve followed my blog for long, you’ll know that tongue & lip ties and nursing challenges are a passion of mine, especially after having experienced challenges with all of these factors with several of my own children. I’ve also been in contact with many moms who are struggling with nursing issues or fussy babies, and so many times there is a connection to either a tongue or lip tie (or both!). Recently, a mom shared her story in a Facebook Group for Moms that I’m part of. Her story touches on so many of the factors that I have seen and/or experienced, that I contacted her and asked for her permission to share her post with you all. I am so grateful, as Tanisha covers many factors to consider in her story, and I think it will be beneficial for many moms who might be struggling. If you are struggling with nursing issues, I really want to encourage you that you aren’t alone, and that there are answers out there!! And if you resonate with this story, I would love to hear about your experiences! It can help other moms when they can hear first-hand what worked for others in similar situations.
~Kelsey
Now on to our guest post, written earlier this year by Tanisha Gingerich:
**Shared by the author’s permission**
I thought I’d make a post for whoever it might concern, about our journey so far with tongue and lip ties. They are becoming increasingly common it seems, and I thought sharing my experience might be a good way to bring awareness so that any other moms going thru something similar can benefit from (or add to) what I’ve been learning.
A week post partum, I was scabbed from nursing, and in a lot of pain every time I fed Micoma. She was gaining well, so we probably could have made it work (a lactation consultant can help you and baby work past a multitude of feeding problems), but I knew from experience that although I could “make it work,” my milk supply was going to tank around 4-6 months. Ties can also cause speech, dental, and sleep issues down the road, along with a host of other problems.
So in the interest of short-term pain for the long-term good, I took Micoma in at a week old for a consultation and ended up getting her lip and tongue ties lasered right away so we could begin the healing and retraining process as soon as possible before bad nursing habits were formed.
I cried and prayed over her before they did the 3 minute procedure, and sobbed compulsively while they swaddled her and used a laser to cut the ties open. The woman doing the procedure was a mom too, and was so compassionate and kind with Micoma. Then they left us alone in a cozy room to nurse, and I heaved more sobs as I comforted my baby. Being able to hold and nurse her was probably just as healing for me as it was for her.
Her latch was instantly better. Over the next few days I had to continually remind myself of the long term good, as I did stretches on her wounds. To my relief, the stretches were done in under 30 seconds, and Micoma always recovered quickly… I soon realized she was screaming louder over getting her diaper changed than she was over the oral invasion, so that made me feel better. I told her all the time how brave she was, and gave her every comfort to guide her through the rough patch.
That first week dragged on for me. I hated having to keep stretches in my mind every 4-6 hours even thru the night—got kind of sick with dread thinking about it. I kept Micoma on Tylenol the first 2 days, and again on day 4 when there was a flare up of discomfort. Other than that though, she continued to eat and sleep very normally (not everyone has it so easy, some babies will hardly eat for a day or two, and cry all the time. Thankfully Micoma nursed for comfort, and seemed to tolerate gracefully any discomfort she was feeling). At one week we had a follow up appointment and they said everything was healing well and there was no reattachment. I was so relieved.
By the second week all was routine, and the scars were nearly healed up. Sometimes she wouldn’t even wake up when I did the stretches so I knew they weren’t painful. Currently we have just passed the 3 week mark, which means I can de-escalate the stretches rapidly and they will disappear in a few days. Hooray! One hurdle over. Now on to the next. I had a lactation consultant come at week 3, to help me teach Micoma new nursing/sucking habits. I learned so much!
First of all, babies begin practicing how to suck from week 12 in utero. This is how they build the oral strength they need for nursing. Unfortunately, when a part of their tongue is tied down, they are unable to fully lift and tone those muscles. When they are born and begin nursing, the restrictions to their lip and or/tongue, make it hard or impossible for them to latch correctly or suck efficiently. As a result, nursing is laborious for them. You may hear a “clicking” noise or notice milk dribbling out the sides of their mouth, these are telltale signs. They frequently fall asleep while nursing, just from the strain it, and are unable to properly empty the breast. This can obviously cause low-weight issues, milk supply issues, and severe frustration to the baby. The baby will often resort to chomping or some other measure in an attempt to get milk, resulting it a lot of discomfort or pain for the mom.
But even after ties are released, there is still some work to do. Baby’s latch will probably be better right away, but you’ll need to help hertone her oral muscles and relearn how to suck correctly with the new range of motion in her mouth. I was given a series of simple tongue exercises to do with Micoma every day… they are more like games, and activate her reflexes to get her tongue moving, especially in the places she’s not used to lifting it.
Now, to back up a bit, there are two kinds of ties—lip ties and tongue ties. I’ve also heard of buchal ties (cheeks) but know very little about them at this point. A lip tie is easiest to spot (example of one in comments) and if a lip tie is present, a tongue tie is almost always present too—they tend to go hand in hand. Keep in mind that some care providers are not trained to look for *posterior* tongue ties (these are in the back of the mouth and not as obvious as anterior ones), so those often get missed. Ties vary in severity (where they are attached and how drastically they are affecting function of the lip/tongue. Sometimes it may be negligible).
Next thing I learned, tongue tied babies are notoriously “tight.” The tongue sits at the very top of the spine, and if there are restrictions in the tongue, you will see restrictions all the way down through the body. Sure enough, Micoma is very tight in her shoulder/neck area, has over compensated for it in her lower back, and has tight hips. Once again, I was given a series of simple rhythmic motions and stretches to loosen those areas up and bring everything into alignment. She has a bit of a “C” shape curve when she lies down, that’s another common sign of tongue-tie related tightness. (Pic in comments) I wish I would have known this with my oldest daughter Verona. She was incredibly C-shaped, and these stretches would have loosened up her uncomfortably tight muscles.
Looking back, both of my children before Micoma had ties of some kind. I always had to use a nipple shield with Verona, and I remember Benny getting so angry when I nursed him. My supply going down around 4 months was another telltale sign. Both children despised tummy time, which was most likely because of how tight they were in their neck and lower back. I suspect “ties” is some of why they slept so poorly and aggravated colic symptoms early on… In-efficient nursing brings more air into the stomach and causes gas discomfort/excessive spitting up. And in a very strange twist of fate, if the tongue cannot reach up to the top of the pallet and rest there while sleeping, the top of the mouth becomes domed, crowding teeth and restricting airway. This can lead to mouth breathing, sleep apnea, and dental issues.
Verona’s lip tie comes all the way down between her teeth, which is why she has a gap between her front teeth. Neither of the children seem to be having difficulty eating, speaking, or maintaining good dental hygiene and structure other than that. So I’ll just keep an eye on them, and only resort to doing anything about theirs at this point if I see it’s going to cause them major problems down the road. But I do grieve the suffering we all went thru with months of screaming colicky baby, and the eventual loss of breastfeeding bond. That pain far surpasses whatever me and Micoma went through the last month in laser-correction and recovery.
So for that reason, I would support moms in pursuing tie-releases if you feel it would be beneficial for your baby. As with everything child-related, there is controversy surrounding the issue—whether ties are really a thing, whether they’re a big deal, clipping or lasering, stretches or no stretches. In my case, I saw enough consequences in my last 2 children that I was willing to believe ties affect quality of life enough to warrant a minor surgery. Lasering has a lower rate of re-attachment and requires no stitches, so I went that route. And the stretches I did because Micoma tolerated them well and I was determined not to let the fibers re-attach while they were healing… and I grilled my caretaker about whether it was necessary, and she says she does see a fairly high rate of reattachment if stretches are not done. Albeit, I did the bare minimum I thought I could be get by with, and with good results. That was my story, you get to write your own. Decide what’s best for your child, whether that’s therapy to work past a tie, or a surgery to correct it, or whatever and don’t let people throw a lot of shame or fear onto you for it.
Currently I am pumping a few times a day and using an SNS (supplemental nursing system) several times a day to stimulate my supply and simultaneously get Micoma the extra food she sometimes can’t get herself. I’ll keep working with Micoma’s body and tongue to get everything loosened up and toned… hopefully within a month we’ll be at a place where she can keep my supply up on her own. In the mean time we’re not goning to go many places this month, just stay home and focus on the task at hand.
Many people take their children to chiropractors pre and/or post tie release for body work. It helps with nursing if your baby is aligned properly. For the time being, since I have bodywork I can do at home with her, I am skipping that… see if I can get by without it. Cranial Sacral therapy is another thing highly recommended… I don’t know, it could possibly be a legitimate thing with babies since their skulls are still un-fused and somewhat mobile, but I have heard of enough occultist ties connected to this practice done in adults that I plan to avoid it all together.
This post was not meant to diagnose or treat any illness. It’s my personal story and some things I learned along the way, left here for people to sift thru and take whatever is for them.
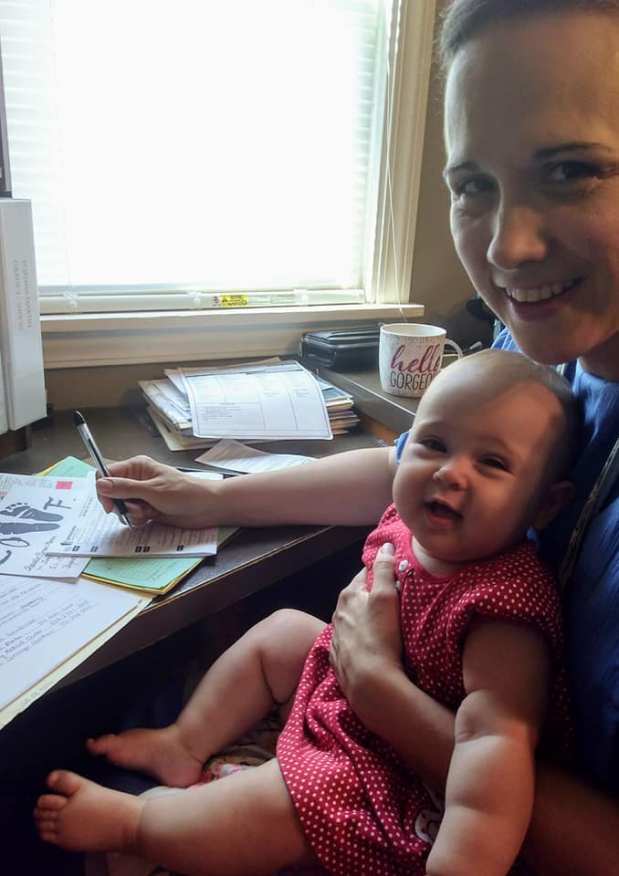
If, btw, you decide lasering is the right option for you (and you are local to central PA), I had a good experience with Dr. Katherman in York. Her office felt like such a warm and caring place to me, and she was on call at all hours if I had questions later. Also, do yourself a favor and hire a lactation consultant. You won’t regret it! Do a bit of research first and find one that people you know have had good experiences with (there are a few bad eggs out there). Again, I had a wonderful experience with the one I found, and I’ll link her website for reference.
Dr Katherman: https://www.cdepa.com
Jessica, Lactation Consultant: https://bornandfed.com
The cost to get two ties lasered was $750. I am going to turn it into my insurance sharing plan, but I do not know yet if they will cover it. The lactation consultant fee for an hour and a half session was $175. So it is a good chunk of change. But when compared to the potential costs of not doing it, it is a very reasonable investment.
I hope that’s everything. My mind is still kind of whirling from all the things I’m learning, so this was my way of processing it. Hoping it will be helpful to someone else.
P.S. Out of curiosity, I asked both the doctor and lactation consultant if ties have become more common recently or if they’re just being diagnosed more, so we’re more aware of them. They both said ties are becoming increasingly common. I don’t think even my mom’s generation would have seen very many, so this seems to be a rapidly developing problem. Presumably, Western diet and lifestyle as well as the declining quality of foods (grown from nutrient-depleted soils) plays a role. There seems to be evidence to support that lack of folate and other B vitamins in the early stages of embryonic development contributes to ties forming—or the presence of the synthetic B vitamin folic acid commonly in prenatals and fortified foods. And others say there are indications that genetic mutations (the MTHFR gene) play a role. But no definitive studies have been done, that I know of. Everything is speculation at this point. Someone gave me two articles so I’m linking them below. My midwife gave me some resources to dig into and I’m hoping to do more research to see if this plague is avoidable.
Connection to MTHFR gene: https://www.checkupnewsroom.com/a-pediatricians-goes-in…/
Connection to regular folic acid intake: https://pubmed.ncbi.nlm.nih.gov/31835174/
I maintain a decently healthy diet and take quality supplements including methylated B vitamins so it’s hard to believe that was the cause of all 3 children having ties. Except that I was under exponential stress the past few years, and as I understand it B vitamins are created in the gut… if you have bad gut health or are under stress, B vitamins do not form well. So that could be a factor. Like I said, I’m going to keep digging and see what answers I can find.