Proactive Preparation Tips: Helping You Achieve a Successful Vaginal Birth
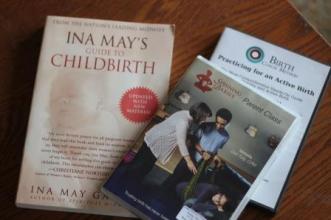
If you’ve read much about preparing for birth, you probably have realized that there tends to be two different “extremes” when it comes to how much or how little you do to prepare your body for the marathon of birth. On the one hand, there are those who feel strongly that you need to “trust your body” to do what it was made to do, and that the addition of herbs and other proactive methods give moms a sense that their body is broken and unable to work on it’s own. The other hand tends to view the whole process of labor and birth as an “accident waiting to happen”, and rushes to medicalize every situation (for example, routinely inducing labor at 41 weeks just because it’s a week past your due date).
My personal opinion (and take this as my opinion-as with anything, you must do your own research and make your own decisions about these suggestions!), is that there should be a balance between these two extremes. I feel strongly that a women’s body was designed to grow, nourish, carry and deliver a baby, and that you can have confidence that this a totally normal and natural process (and not a medical emergency!). But just like any other capabilities your body may have, these abilities can be supported, enhanced and enabled to do their job more efficiently, smoothly and successfully. With that mindset, I’m going to share with you some suggestions on how to support and prepare your body in order to provide you with a greater possibility of achieving a low-risk, normal, natural vaginal birth.
Some of the biggest factors that arise that prevent moms from their desired birth outcome include: pain in pregnancy that prevent them from moving well at the end of pregnancy, going so far past your due date that your care provider feels like an induction is necessary, a long early phase of labor that prevents mom from getting adequate rest and results in exhaustion (which often ends in transport from home and/or an epidural to provide needed relaxation), and a long pushing period that sometimes ends in surgical or assisted delivery. While there are varying factors in all of these situations that can all be prevented, there are MANY things you can do to reduce your risk of these situations occurring, if you just know what to be aware of and how to help your body to prepare!
- Movement, Alignment and Positioning:
One key factor that makes a difference in your pregnancy comfort level, baby’s ability to descend efficiently, and your overall length of pregnancy/labor is the position of your baby in relation to your pelvis. I highly recommend you find a good chiropractor in your area (for those who are local you can find some recommendations when you click on the “Local Resources” tab) who is certified in Webster technique and works with pregnant moms, and get regular adjustments specifically throughout the last 6 weeks of pregnancy. If your pelvis and muscles are out of alignment, they can keep baby from being able to descend into a position that is optimal for triggering the start of labor, and the ability of the baby to navigate the birth canal, which can then cause labor to stall and/or make it more challenging for you during the pushing phase.
For the best explanation of position and how this can affect labor (and what you can do about it!), I highly recommend that you take the time to watch the Parent Class taught by Gail Tully at Spinning Babies. Once you’ve watched it, check out the Spinning Babies website for more tips and suggestions on optimizing your baby’s position. And finally, if you are getting near your due date (or are past your due date and are waiting for baby!), taking time to complete a few rounds of the Miles Circuit exercises has been shown to improve baby’s position and encourage labor to happen.
- Exercise:
As they say, you don’t decide to run a marathon and then complete it tomorrow! I think it’s wise to go into labor with a similar mindset as one would in preparing for a long-distance athletic event. Regular exercises that help to strengthen your legs, open your pelvis (think deep squats and lunges) and build your stamina can play a role in encouraging baby to come in good time, helping to improve your ability to handle the rigors of labor and provide you with a much better recovery. Even if you’re only able to include ten minutes of purposeful exercise a day, it will give you great benefits. Here’s one to get you started: 10 Minute Pregnancy Workout. Long, brisk walks and swimming are also great exercises to consider including in yoaur routine.
- Herbal Supplements:
- Red Raspberry Leaf Tea has amazing health benefits, besides helping to prepare and tone your uterus making contractions more efficient. I have more information on this great tea in my post over here, and you can begin drinking one cup a day during the 2nd trimester, increasing to 3+ cups per day as you near your due date.
- Birth Preparation Formula: I have personally had great success taking an herbal supplement during the last 5-6 weeks of my pregnancies that is specifically geared towards preparing your uterus and cervix for labor. Yes, I take it in addition to Red Raspberry Leaf tea. If you have a history of preterm birth, you would want to wait to start this until 36 weeks, and on the flip side, if you tend to go way past your due date, you could begin taking it at 34 weeks up until delivery. The moms that I have had take this tend to have shorter labors, earlier deliveries, and minimal postpartum bleeding (myself included!). There are several different brands available, though I tend to think the tincture forms work the best. My all-time favorite is the Gentle Birth Formula. You will need 4 to 6oz in order to take it daily for 5-6 weeks, and it’s best to not consume the tincture in the late afternoon/evening, as it can cause contractions that may prevent you from sleeping!
- Evening Primrose Oil or Borage Oil: The high GLA content in either of these oils can help to soften and prepare your cervix for labor, which can assist the body in working more efficiently once labor actually begins. You want a “mega” gel-cap with 1000mg or more per capsule, and this can be taken orally every day for the last trimester, and then also inserted vaginally at bedtime during the last few weeks of pregnancy.
- Abdominal Support:
Some moms just need some extra support for their abdominal muscles, especially if they have had a few babies, or if their babies tend to be large. The muscles that support the uterus and help it to contract efficiently can become stretched (think of a rubberband that has been completely stretched out, and doesn’t quite return to “normal”), and are unable to “hug” baby enough to get a consistent labor pattern started, or even get baby low enough to obtain a good position to begin with! One way to work with this is to consider regularly providing your uterus with support, in particularly during the last 6-8 weeks of pregnancy. You can purchase a maternity support belt (Belly Bandit has some great, albeit expensive options), but many women find that using a rebozo or long scarf/piece of scarf works great, such as is illustrated in this post here and another option here. The goal is to pull the uterus slightly up and towards you, mimicking the way your muscles naturally pull, with provides a firm, consistent support (which also relieves pressure from your back!).
- Eating Dates!
The benefit of consuming dates during the last weeks of pregnancy has only recently been discovered. The suggested protocol is to eat 4-6 dates daily beginning around 36 weeks until you deliver. To find out more, you can check out the details of a recent study at Evidence Based Birth and see what Mama Natural has to say here.
With the exception of eating dates (this is newer option I’ve discovered!), I have personally tried all of the above suggestions for my own five pregnancies and births, and have seen many women successfully use these recommendations throughout my midwifery practice over the past 11+ years. I wish I would have known about many of these earlier in my practice, as I think it would have prevented more transfers and unnecessarily lengthy labors. Another side benefit to following these suggestions is that your body is that much more prepared and ready should an induction actually be medically indicated. While I rarely have reason to need to get labor started, when there is this need and the body is ready for labor, then there are many more options available that have a high likelihood of actually working (in case you’re wondering, one method many midwives use is the Midwife’s Brew, but you should never attempt this without discussing the details, risk vs. benefit, etc. with your care provider!). And if you end up needing a hospitalized induction, the above suggestions will also increase the chances that you end up with a successful induction and normal vaginal birth.








 This experience has been different yet! The first few weeks found baby gaining really slowly (she lost a pound after birth, and took three weeks to regain it!), which of course had me worried after everything that happened with my previous baby. But around 3 weeks old, things began to shift, and her suck got stronger and she began to gain weight! By now, at 7 weeks, she is a healthy, chunky 11 pounds, which means she has put on 2 pounds in just over 2 weeks! I thought perhaps there might be some other moms out there looking for ways to increase and improve their milk supply, so I’m going to share some of my favorite suggestions…some of these I found helpful when I was exclusively pumping for baby #4, and they have gone on to be helpful this time around.
This experience has been different yet! The first few weeks found baby gaining really slowly (she lost a pound after birth, and took three weeks to regain it!), which of course had me worried after everything that happened with my previous baby. But around 3 weeks old, things began to shift, and her suck got stronger and she began to gain weight! By now, at 7 weeks, she is a healthy, chunky 11 pounds, which means she has put on 2 pounds in just over 2 weeks! I thought perhaps there might be some other moms out there looking for ways to increase and improve their milk supply, so I’m going to share some of my favorite suggestions…some of these I found helpful when I was exclusively pumping for baby #4, and they have gone on to be helpful this time around.













 Before I had children, I would have said that breastmilk is the absolute best choice for feeding a baby, and that a mom should try everything possible to breastfeed…and that if you tried hard enough, you would be able to succeed. However, once I entered the realm of motherhood, and actually experienced the things I had only previously read/observed/seen, I have learned that ideals are not always reality. My youngest baby just turned 10 months old, and I have once again faced the challenges of tongue-ties, latch issues, lack of sufficient supply, colic, fussiness, food sensitives, and more. Some of those subjects will be material for future posts, but I mention them to give you the background as to what inspired this post. As we have worked through these challenges, my husband has encouraged me that perhaps the things we learned will benefit others, so this is an attempt to do just that!
Before I had children, I would have said that breastmilk is the absolute best choice for feeding a baby, and that a mom should try everything possible to breastfeed…and that if you tried hard enough, you would be able to succeed. However, once I entered the realm of motherhood, and actually experienced the things I had only previously read/observed/seen, I have learned that ideals are not always reality. My youngest baby just turned 10 months old, and I have once again faced the challenges of tongue-ties, latch issues, lack of sufficient supply, colic, fussiness, food sensitives, and more. Some of those subjects will be material for future posts, but I mention them to give you the background as to what inspired this post. As we have worked through these challenges, my husband has encouraged me that perhaps the things we learned will benefit others, so this is an attempt to do just that!




 midwifery is her calling, so she’s hoping to attend births in January (as long as babies give her enough time to get here!). We’ll see where things go, but we’re excited to have Charity join our team this month!
midwifery is her calling, so she’s hoping to attend births in January (as long as babies give her enough time to get here!). We’ll see where things go, but we’re excited to have Charity join our team this month!